Diabetes 2 Etiology refers to the study of the causes and risk factors associated with the development of type 2 diabetes. Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels due to the body’s ineffective use of insulin.
Understanding the etiology of diabetes 2 is crucial for effective prevention and management strategies. Risk factors include age, genetics, obesity, physical inactivity, unhealthy diet, and family history. Research in diabetes 2 etiology has led to significant advancements in identifying modifiable risk factors, allowing for targeted interventions to reduce the incidence and progression of the disease.
Further exploration of diabetes 2 etiology involves examining the complex interplay between genetic, environmental, and behavioral factors. Ongoing research aims to unravel the mechanisms underlying the development of type 2 diabetes, leading to improved diagnostic tools, personalized treatment plans, and ultimately, better outcomes for individuals affected by this condition.
Diabetes 2 Etiology
Understanding the etiology of diabetes 2 is crucial for effective prevention and management strategies. Key aspects to consider include:
- Genetics: Family history and genetic variants play a role.
- Obesity: Excess weight increases insulin resistance.
- Age: Risk increases with age, especially over 45.
- Physical Inactivity: Lack of exercise contributes to insulin resistance.
- Diet: Unhealthy diets high in processed foods and sugary drinks increase risk.
- Ethnicity: Certain ethnic groups have a higher prevalence of diabetes 2.
- Metabolic Syndrome: A cluster of conditions (obesity, high blood pressure, high cholesterol, high blood sugar) increases risk.
These aspects are interconnected. For example, obesity can lead to physical inactivity, which further increases insulin resistance. Additionally, unhealthy diets often accompany obesity, creating a vicious cycle that promotes the development of diabetes 2. Understanding these connections is essential for developing comprehensive strategies to prevent and manage this condition.
Genetics
The connection between genetics and diabetes 2 etiology is significant. Family history, indicating a genetic predisposition, and specific genetic variants are both risk factors for developing type 2 diabetes.
- Genetic Predisposition: A family history of diabetes 2 suggests an inherited susceptibility to the condition. Studies have identified specific genes linked to an increased risk of developing type 2 diabetes.
- Genetic Variants: Researchers have identified genetic variants, known as single nucleotide polymorphisms (SNPs), associated with an increased risk of diabetes 2. These variants can affect various genes involved in insulin secretion, insulin action, and glucose metabolism.
- Gene-Environment Interactions: Genetic factors interact with environmental factors, such as diet and lifestyle, to influence the development of diabetes 2. For example, individuals with a genetic predisposition to diabetes may be more susceptible to the effects of an unhealthy diet or physical inactivity.
Understanding the genetic basis of diabetes 2 etiology has implications for prevention and management. Identifying individuals at high risk based on their family history and genetic variants allows for targeted interventions, such as lifestyle modifications and early screening, to delay or prevent the onset of the disease.
Obesity
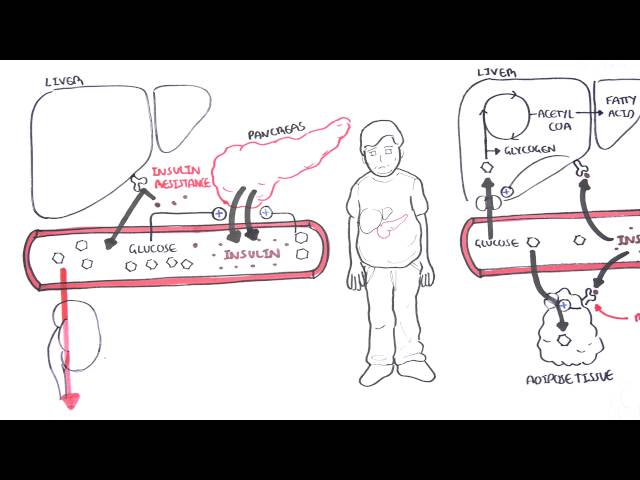
Obesity is a major risk factor for developing type 2 diabetes. Excess weight, particularly around the abdomen, leads to insulin resistance, a condition in which the body’s cells do not respond effectively to insulin. Insulin is a hormone produced by the pancreas that helps glucose, or sugar, enter cells for energy production.
When cells become insulin resistant, glucose builds up in the bloodstream, leading to high blood sugar levels. Over time, high blood sugar can damage blood vessels and organs, increasing the risk of heart disease, stroke, kidney disease, and blindness.
Obesity contributes to insulin resistance through several mechanisms. Excess weight puts stress on the pancreas, making it difficult to produce enough insulin. Additionally, fat cells release hormones that interfere with insulin signaling, further reducing insulin sensitivity.
Understanding the connection between obesity and insulin resistance is crucial for preventing and managing type 2 diabetes. Maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce the risk of developing insulin resistance and its associated complications.
Age
The relationship between age and diabetes 2 etiology is well-established. As we age, our risk of developing type 2 diabetes increases, particularly after the age of 45. Several factors contribute to this age-related risk:
- Decreased Insulin Sensitivity: With age, the body becomes less sensitive to insulin, meaning that more insulin is required to lower blood sugar levels.
- Reduced Beta-Cell Function: The pancreas produces insulin through beta cells. As we age, the number and function of beta cells decline, leading to decreased insulin production.
- Increased Inflammation: Chronic inflammation is associated with aging and can contribute to insulin resistance and the development of type 2 diabetes.
- Changes in Body Composition: Age-related changes in body composition, such as increased fat mass and decreased muscle mass, can also contribute to insulin resistance.
Understanding the connection between age and diabetes 2 etiology is crucial for developing targeted prevention and management strategies. Regular monitoring of blood sugar levels, maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet can help reduce the risk of developing type 2 diabetes, even as we age.
Physical Inactivity
Physical inactivity is a significant contributor to insulin resistance, a condition in which the body’s cells do not respond effectively to insulin. Insulin is a hormone produced by the pancreas that helps glucose, or sugar, enter cells for energy production. When cells become insulin resistant, glucose builds up in the bloodstream, leading to high blood sugar levels. Over time, high blood sugar can damage blood vessels and organs, increasing the risk of heart disease, stroke, kidney disease, and blindness.
Regular physical activity improves insulin sensitivity and helps control blood sugar levels. Exercise stimulates the muscles to take up glucose from the bloodstream, even without insulin. Additionally, exercise helps reduce body fat, which is associated with improved insulin sensitivity. Conversely, physical inactivity leads to decreased muscle mass and increased body fat, both of which contribute to insulin resistance.
Understanding the connection between physical inactivity and insulin resistance is crucial for preventing and managing type 2 diabetes. Regular physical activity, such as brisk walking, cycling, or swimming for at least 30 minutes most days of the week, can significantly reduce the risk of developing insulin resistance and its associated complications.
Diet
Unhealthy diets high in processed foods and sugary drinks are major contributors to the development of type 2 diabetes. Processed foods often contain high levels of unhealthy fats, sodium, and added sugars, all of which can contribute to weight gain and insulin resistance. Sugary drinks, such as soda, fruit juice, and energy drinks, provide empty calories and can lead to rapid spikes in blood sugar levels.
Consuming a diet high in processed foods and sugary drinks can lead to several health issues that increase the risk of developing type 2 diabetes. For example, obesity, a major risk factor for type 2 diabetes, is often caused by a diet high in processed foods and sugary drinks. Additionally, unhealthy diets can lead to high blood pressure, high cholesterol, and inflammation, all of which are associated with an increased risk of type 2 diabetes.
Understanding the connection between diet and diabetes 2 etiology is crucial for developing effective prevention and management strategies. By making healthier food choices, such as consuming more fruits, vegetables, and whole grains, and limiting the intake of processed foods and sugary drinks, individuals can significantly reduce their risk of developing type 2 diabetes and its associated complications. Health professionals play a vital role in educating the public about the importance of healthy eating habits and promoting dietary interventions to prevent and manage type 2 diabetes.
Ethnicity
The connection between ethnicity and diabetes 2 etiology is complex and multifaceted. Certain ethnic groups exhibit a higher prevalence of diabetes 2, influenced by a combination of genetic, environmental, and sociocultural factors.
- Genetic Predisposition: Some ethnic groups may have a higher prevalence of specific genetic variants associated with an increased risk of developing diabetes 2.
- Environmental Factors: Environmental factors, such as dietary habits, physical activity levels, and access to healthcare, can vary significantly among different ethnic groups and influence the risk of diabetes 2.
- Sociocultural Factors: Sociocultural factors, such as cultural beliefs, dietary practices, and healthcare-seeking behaviors, can also contribute to the higher prevalence of diabetes 2 in certain ethnic groups.
- Disparities in Healthcare Access and Quality: Disparities in healthcare access and quality can lead to delayed diagnosis, inadequate treatment, and poorer outcomes for individuals from certain ethnic groups.
Understanding the complex interplay between ethnicity and diabetes 2 etiology is crucial for developing targeted interventions and policies to address health disparities and improve outcomes for all individuals at risk of developing diabetes 2.
Metabolic Syndrome
Metabolic syndrome refers to a group of conditions that occur together, increasing the risk of developing diabetes 2 and cardiovascular diseases. Understanding the connection between metabolic syndrome and diabetes 2 etiology is crucial for effective prevention and management strategies.
- Obesity: Excess weight, particularly around the abdomen, is a major component of metabolic syndrome. Obesity leads to insulin resistance, a condition in which the body’s cells do not respond effectively to insulin, resulting in high blood sugar levels.
- High Blood Pressure: Hypertension, or high blood pressure, is another component of metabolic syndrome. High blood pressure can damage blood vessels and increase the risk of heart disease and stroke.
- High Cholesterol: Elevated levels of cholesterol, particularly LDL (bad) cholesterol, are associated with metabolic syndrome. High cholesterol can contribute to the formation of plaques in arteries, increasing the risk of heart disease and stroke.
- High Blood Sugar: Impaired glucose metabolism, characterized by high blood sugar levels, is a central feature of metabolic syndrome. High blood sugar can damage blood vessels and organs, leading to complications such as heart disease, stroke, kidney disease, and blindness.
The presence of multiple components of metabolic syndrome significantly increases the risk of developing diabetes 2. Individuals with metabolic syndrome are more likely to have insulin resistance, impaired glucose metabolism, and other factors that contribute to the development of type 2 diabetes.
FAQs on Diabetes 2 Etiology
This section addresses common questions and misconceptions surrounding the causes and risk factors associated with type 2 diabetes (diabetes 2), providing concise and informative answers based on current scientific understanding.
Question 1: What is the main cause of diabetes 2?
Answer: Diabetes 2 is primarily caused by a combination of genetic and environmental factors. It develops when the body becomes resistant to insulin or does not produce enough insulin, leading to high blood sugar levels.
Question 2: What are the major risk factors for developing diabetes 2?
Answer: Key risk factors include obesity, physical inactivity, unhealthy diet, family history of diabetes, advancing age, and certain ethnicities.
Question 3: Is diabetes 2 preventable?
Answer: While genetic predisposition plays a role, lifestyle modifications can significantly reduce the risk of developing diabetes 2. Maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet are crucial preventive measures.
Question 4: What are the long-term consequences of untreated diabetes 2?
Answer: Uncontrolled diabetes 2 can lead to severe complications, including heart disease, stroke, kidney failure, blindness, and nerve damage.
Question 5: How is diabetes 2 diagnosed?
Answer: Diagnosis involves blood tests that measure blood sugar levels, such as the fasting blood glucose test or the oral glucose tolerance test.
Question 6: What are the treatment options for diabetes 2?
Answer: Treatment plans typically include a combination of lifestyle changes, oral medications, and in some cases, insulin therapy. Regular monitoring of blood sugar levels is essential for effective management.
Summary: Understanding the etiology of diabetes 2 empowers individuals to take proactive steps towards prevention and management. Through healthy lifestyle choices and regular medical check-ups, the risk of developing and experiencing complications from diabetes 2 can be significantly reduced.
Next Section: Living with Diabetes 2: Management and Support
Diabetes 2 Etiology
Understanding the etiology of diabetes 2 is crucial for effective prevention and management. Here are some practical tips to mitigate risk and improve outcomes:
Tip 1: Maintain a Healthy Weight
Excess weight, particularly around the abdomen, increases the risk of insulin resistance and type 2 diabetes. Aim for a healthy body mass index (BMI) and reduce waist circumference through a balanced diet and regular exercise.
Tip 2: Engage in Regular Physical Activity
Regular exercise improves insulin sensitivity and helps control blood sugar levels. Engage in at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week.
Tip 3: Adopt a Balanced Diet
Focus on consuming a diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats to prevent weight gain and improve blood sugar control.
Tip 4: Get Regular Medical Check-ups
Regular medical check-ups allow healthcare professionals to monitor blood sugar levels, assess risk factors, and provide timely interventions to prevent or manage diabetes 2.
Tip 5: Quit Smoking
Smoking damages blood vessels and increases the risk of diabetes 2 and its complications. Quitting smoking is essential for overall health and diabetes prevention.
Tip 6: Manage Stress
Chronic stress can elevate blood sugar levels and increase insulin resistance. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Tip 7: Get Enough Sleep
Lack of sleep can disrupt hormone regulation and increase the risk of insulin resistance. Aim for 7-8 hours of quality sleep each night.
Tip 8: Limit Alcohol Consumption
Excessive alcohol consumption can contribute to weight gain, insulin resistance, and high blood sugar levels. Drink alcohol in moderation or consider avoiding it altogether.
Summary: By incorporating these tips into your lifestyle, you can significantly reduce your risk of developing diabetes 2 or manage the condition effectively if you have it. Remember, prevention is always better than cure. Early intervention and lifestyle modifications are key to maintaining good health and well-being.
Next Section: Understanding the Impact of Diabetes 2 on Overall Health
Conclusion
Understanding the etiology of diabetes 2 is paramount in developing effective strategies for prevention, management, and treatment. This article has explored the complex interplay of genetic, environmental, and lifestyle factors that contribute to the development of this condition.
The key takeaway is that diabetes 2 is largely preventable through lifestyle modifications, including maintaining a healthy weight, engaging in regular physical activity, adopting a balanced diet, and quitting smoking. Regular medical check-ups are crucial for early detection and intervention. For those diagnosed with diabetes 2, proper management is essential to mitigate the risk of complications and maintain overall well-being.
Future research endeavors should continue to unravel the intricacies of diabetes 2 etiology, leading to the discovery of novel therapeutic targets and improved outcomes for individuals affected by this condition. By raising awareness and promoting healthy lifestyle choices, we can collectively work towards reducing the burden of diabetes 2 and its associated complications.
Youtube Video: