In the context of managing diabetes, the term “shots” refers to injections of insulin or other medications delivered subcutaneously using a syringe or an insulin pen. Insulin is a naturally occurring hormone responsible for regulating glucose levels in the body. Individuals with diabetes may require insulin injections to supplement or replace their body’s insufficient insulin production. These shots help control blood sugar levels, preventing complications associated with diabetes, such as nerve damage, kidney disease, and vision problems.
Insulin therapy has been a cornerstone in diabetes management since its discovery in the 1920s. Over the years, advancements in insulin formulations and injection methods have significantly improved the efficacy, convenience, and overall quality of life for people living with diabetes. Modern insulin analogs, with their extended duration of action and reduced risk of hypoglycemia, offer greater flexibility and better control. Furthermore, the development of insulin pens and other user-friendly injection devices has made self-administration easier and less daunting.
Understanding the principles of insulin therapy, proper injection techniques, and regular monitoring of blood sugar levels are essential for successful diabetes management. Healthcare professionals play a crucial role in educating and supporting individuals with diabetes, empowering them to make informed decisions about their treatment plans. Insulin shots, combined with a balanced diet, regular exercise, and other lifestyle modifications, can effectively manage diabetes, allowing individuals to lead healthy and fulfilling lives.
shots for diabetes
In the context of diabetes management, “shots” primarily refer to insulin injections, which are essential for regulating blood sugar levels. These injections involve various key aspects that contribute to their effectiveness and overall impact on diabetes care.
- Insulin: A hormone that regulates glucose metabolism, injected to supplement or replace the body’s own production.
- Subcutaneous: The layer of tissue beneath the skin, where insulin is injected for absorption.
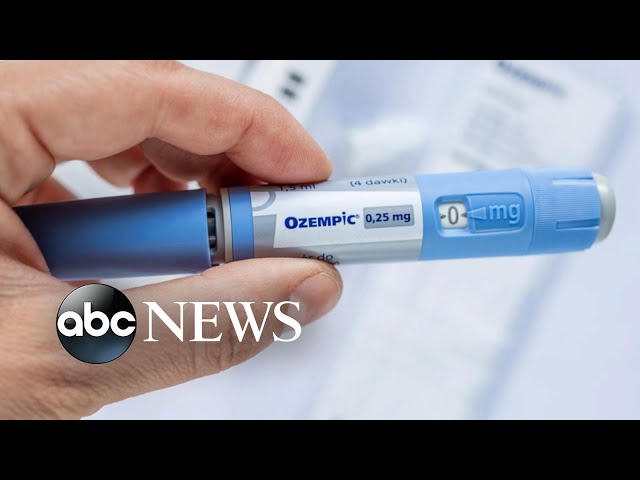
- Syringe or Pen: Devices used to deliver insulin injections.
- Blood Sugar Control: The primary goal of insulin shots, to prevent complications associated with diabetes.
- Convenience: Modern injection methods, such as insulin pens, offer ease and flexibility in self-administration.
- Education: Healthcare professionals play a vital role in educating individuals on insulin therapy and injection techniques.
- Monitoring: Regular blood sugar monitoring is crucial to assess the effectiveness of insulin shots.
- Lifestyle Modifications: Insulin shots work in conjunction with a balanced diet, exercise, and other lifestyle changes for optimal diabetes management.
These key aspects highlight the multifaceted nature of insulin shots in diabetes care. From the hormone itself to the methods of administration and the importance of education and monitoring, each aspect contributes to the successful management of diabetes and the well-being of individuals living with this condition.
Insulin
Insulin is a hormone produced by the pancreas, responsible for regulating glucose metabolism in the body. It facilitates the uptake of glucose from the bloodstream into cells, where it is utilized for energy or stored for later use. In individuals with diabetes, the body either does not produce enough insulin or does not use insulin effectively, leading to elevated blood sugar levels.
Insulin injections, commonly referred to as “shots for diabetes,” play a crucial role in managing blood sugar levels and preventing complications associated with diabetes. By supplementing or replacing the body’s own insulin production, these injections help regulate glucose metabolism, ensuring that cells receive the energy they need to function properly.
The connection between insulin and shots for diabetes is evident in the fact that insulin is the primary active component of these injections. Without insulin, individuals with diabetes would not be able to effectively control their blood sugar levels, highlighting the importance of insulin as a component of shots for diabetes.
In practical terms, understanding the connection between insulin and shots for diabetes empowers individuals to make informed decisions about their treatment plans. It reinforces the need for adherence to prescribed insulin regimens and regular blood sugar monitoring to ensure optimal management of diabetes.
In conclusion, insulin, as a hormone regulating glucose metabolism, is central to the mechanism of action of shots for diabetes. Insulin injections provide a means to supplement or replace the body’s own insulin production, enabling individuals with diabetes to manage their blood sugar levels effectively and maintain their overall well-being.
Subcutaneous
Subcutaneous injection, a technique commonly used in administering shots for diabetes, involves delivering insulin into the subcutaneous layer of tissue beneath the skin. This specific layer is targeted for insulin injection due to several factors that contribute to the effectiveness and safety of this method.
- Absorption Rate: The subcutaneous layer provides a consistent and reliable absorption rate for insulin, ensuring predictable and sustained insulin delivery into the bloodstream.
- Reduced Pain: Compared to intramuscular or intravenous injections, subcutaneous injections cause less pain and discomfort due to the lower density of nerve endings in the subcutaneous tissue.
- Fewer Blood Vessels: The subcutaneous layer has fewer blood vessels compared to other injection sites, reducing the risk of bleeding or hematoma formation.
- Self-Administration: Subcutaneous injections can be easily self-administered, empowering individuals with diabetes to manage their condition conveniently and independently.
The connection between subcutaneous injection and shots for diabetes lies in the fact that the subcutaneous layer serves as the primary site for insulin delivery in this context. The properties of the subcutaneous tissue, such as its absorption rate, pain profile, and accessibility, make it an ideal location for insulin injections. Understanding this connection enables individuals with diabetes to have a better grasp of their treatment plans and the rationale behind the chosen injection method.
Syringe or Pen
In the context of shots for diabetes, the choice between a syringe or pen for insulin injection depends on various factors such as individual preferences, dexterity, and treatment regimen. Both devices have their own advantages and disadvantages, which should be considered when making a decision.
- Convenience: Insulin pens are generally considered more convenient and user-friendly compared to syringes. They are pre-filled with insulin, eliminating the need for measuring and drawing insulin from a vial. Pens are also more compact and discreet, making them easier to carry and use in public settings.
- Accuracy: Syringes offer greater precision in insulin dosing, as the user can manually adjust the amount of insulin being injected. This level of control may be preferred by individuals who require very specific or flexible insulin doses.
- Cost: Syringes are generally less expensive than insulin pens. However, the cost of insulin pens may be offset by their convenience and ease of use for some individuals.
- Disposability: Insulin pens are typically disposable, while syringes can be reused after proper cleaning and sterilization. This can be a consideration for individuals who prefer a more environmentally friendly option.
Ultimately, the choice between a syringe or pen for shots for diabetes is a personal one. Individuals should consult with their healthcare provider to determine which device is most appropriate for their specific needs and preferences.
Blood Sugar Control
Insulin shots, commonly used in diabetes management, play a crucial role in regulating blood sugar levels to prevent the onset and progression of diabetes-related complications. Understanding the connection between blood sugar control and shots for diabetes is essential for effective disease management.
- Maintaining Blood Sugar Levels: Insulin shots help maintain blood sugar levels within a healthy range, preventing both high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia).
- Preventing Long-Term Complications: Sustained high blood sugar levels can lead to severe complications such as heart disease, stroke, kidney disease, and nerve damage. Insulin shots help prevent these complications by keeping blood sugar levels under control.
- Improving Quality of Life: Managing blood sugar levels through insulin shots can significantly improve an individual’s quality of life by reducing the risk of debilitating complications and promoting overall well-being.
- Empowering Individuals: Insulin shots empower individuals with diabetes to take an active role in their health management. By administering shots as prescribed, they can maintain blood sugar control and reduce the likelihood of complications.
In conclusion, insulin shots are intricately connected to blood sugar control in diabetes management. Their primary goal is to maintain healthy blood sugar levels, thereby preventing the onset and progression of diabetes-related complications. Understanding this connection empowers individuals with diabetes to make informed decisions about their treatment plans and actively participate in their own health journey.
Convenience
In the realm of diabetes management, convenience plays a pivotal role in ensuring adherence to treatment plans and empowering individuals to take charge of their health. Modern injection methods, such as insulin pens, have revolutionized the delivery of insulin shots, making them more convenient, user-friendly, and adaptable to various lifestyles.
- Pre-filled Dosing: Insulin pens eliminate the need for manual measuring and drawing of insulin from vials, reducing the risk of dosage errors and simplifying the injection process.
- Compact and Discreet: Insulin pens are designed to be compact and discreet, allowing for discreet administration in public or social settings without drawing undue attention.
- Flexibility and Portability: Insulin pens offer greater flexibility and portability compared to traditional syringes. They can be easily carried in pockets, bags, or backpacks, enabling individuals to administer their insulin shots on the go.
- Reduced Pain and Discomfort: Insulin pens are engineered with fine needles and injection mechanisms that minimize pain and discomfort during injection, making the experience less daunting for users.
The convenience offered by modern injection methods like insulin pens has a profound impact on the lives of individuals with diabetes. It empowers them to manage their condition more effectively, reduces the burden of treatment, and improves their overall quality of life. By making insulin shots more convenient and accessible, these advancements play a crucial role in promoting adherence to treatment plans and optimizing diabetes management.
Education
In the context of diabetes management, education serves as a cornerstone, empowering individuals to understand their condition, treatment options, and self-care practices. Healthcare professionals, including doctors, nurses, and diabetes educators, play a pivotal role in providing comprehensive education on insulin therapy and injection techniques, ensuring optimal outcomes for individuals with diabetes.
The connection between education and shots for diabetes is multifaceted. Firstly, proper education equips individuals with the knowledge and skills necessary for successful self-management. They learn about different types of insulin, injection devices, and techniques, enabling them to administer their insulin shots safely and effectively.
Furthermore, education empowers individuals to make informed decisions about their treatment plans. By understanding the principles of insulin therapy, they can work collaboratively with their healthcare team to determine the most appropriate insulin regimen and adjust their doses as needed. This knowledge also enables them to recognize and respond appropriately to potential complications, such as hypoglycemia or hyperglycemia.
Real-life examples underscore the importance of education in insulin therapy. Studies have shown that individuals who receive comprehensive education experience better glycemic control, reduced risk of complications, and improved overall health outcomes. Conversely, inadequate education can lead to incorrect injection techniques, medication errors, and suboptimal diabetes management.
The practical significance of this understanding lies in its direct impact on the lives of individuals with diabetes. By investing in education, healthcare professionals empower them to take ownership of their condition, meningkatkan adherence to treatment plans, and ultimately achieve better health outcomes. This education forms the foundation for successful diabetes management, enabling individuals to live full and active lives.
Monitoring
In the context of diabetes management, monitoring blood sugar levels is an indispensable component of insulin therapy. Regular blood sugar monitoring provides valuable insights into the effectiveness of insulin shots and enables timely adjustments to ensure optimal glycemic control.
The connection between monitoring and shots for diabetes is rooted in the need to evaluate the impact of insulin on blood glucose levels. By measuring blood sugar before and after insulin injections, individuals can assess how their body responds to the medication and identify any discrepancies between the desired and actual outcomes. This information guides dose adjustments and helps prevent both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar).
Real-life examples underscore the significance of blood sugar monitoring in insulin therapy. Studies have shown that individuals who regularly monitor their blood sugar experience better glycemic control and reduced risk of complications. Conversely, inadequate monitoring can lead to missed or delayed insulin adjustments, potentially leading to severe health consequences.
The practical significance of this understanding lies in empowering individuals with diabetes to actively participate in their own health management. By regularly monitoring their blood sugar, they can proactively identify patterns, recognize potential issues, and make informed decisions in collaboration with their healthcare team. This knowledge and self-monitoring capability translate into improved diabetes management outcomes and enhanced quality of life.
In conclusion, monitoring blood sugar levels is an integral part of shots for diabetes, providing essential feedback for effective insulin therapy. Regular monitoring empowers individuals to assess the effectiveness of their insulin shots, make timely adjustments, and ultimately achieve optimal glycemic control.
Lifestyle Modifications
In the context of diabetes management, “shots for diabetes” or insulin injections play a crucial role in regulating blood sugar levels. However, it is important to recognize that insulin therapy alone is not sufficient for optimal diabetes management. Lifestyle modifications, including a balanced diet, regular exercise, and other healthy habits, are essential components of a comprehensive diabetes management plan.
- Balanced Diet: Maintaining a balanced diet is pivotal for managing diabetes. Individuals should focus on consuming nutrient-rich foods such as fruits, vegetables, whole grains, and lean proteins. Limiting processed foods, sugary drinks, and unhealthy fats can help stabilize blood sugar levels and reduce the risk of complications.
- Regular Exercise: Engaging in regular physical activity is another key component of diabetes management. Exercise helps improve insulin sensitivity, allowing the body to use insulin more effectively. Aiming for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week can significantly benefit.
- Weight Management: Maintaining a healthy weight is crucial for individuals with diabetes. Excess weight can contribute to insulin resistance, making it more difficult to control blood sugar levels. Adopting a balanced diet and engaging in regular exercise can help achieve and maintain a healthy weight.
- Stress Management: Stress can have a negative impact on blood sugar control. Techniques such as yoga, meditation, or deep breathing exercises can help manage stress levels and improve overall diabetes management.
In conclusion, while insulin shots are an essential component of diabetes management, they work most effectively in conjunction with a balanced diet, regular exercise, and other healthy lifestyle modifications. Adopting these lifestyle changes can significantly improve glycemic control, reduce the risk of complications, and enhance the overall well-being of individuals with diabetes.
Frequently Asked Questions about “Shots for Diabetes”
This section addresses common questions and concerns regarding the use of insulin injections, or “shots,” in diabetes management, providing clear and informative answers to empower individuals.
Question 1: What is the purpose of insulin shots in diabetes management?
Insulin shots are used to supplement or replace the body’s natural insulin production in individuals with diabetes. Insulin is a hormone that regulates blood sugar levels, and insulin shots help ensure that cells receive the energy they need.
Question 2: How often do I need to take insulin shots?
The frequency of insulin shots depends on the type of diabetes, individual needs, and the specific insulin regimen prescribed by a healthcare professional.
Question 3: Do insulin shots hurt?
Insulin shots are generally well-tolerated, and the pain associated with injections is typically minimal. Modern insulin pens and fine needles are designed to minimize discomfort during administration.
Question 4: Can I take insulin shots on my own?
Yes, with proper training and guidance from a healthcare professional, individuals with diabetes can learn to self-administer insulin shots safely and effectively.
Question 5: What should I do if I miss an insulin shot?
If you miss an insulin shot, it is important to take it as soon as possible. Do not double the dose to make up for the missed shot, as this can lead to dangerously low blood sugar levels.
Question 6: How can I manage the side effects of insulin shots?
Common side effects of insulin shots include low blood sugar (hypoglycemia) and weight gain. Regular blood sugar monitoring and working closely with a healthcare professional can help manage these side effects.
Understanding these FAQs can empower individuals with diabetes to take an active role in their own health management and optimize the use of insulin shots for effective blood sugar control.
Transition to the next article section: Insulin shots are an integral part of diabetes management, but they work most effectively when combined with a healthy lifestyle that includes a balanced diet, regular exercise, and stress management. Exploring these aspects in more detail can provide a comprehensive understanding of diabetes management.
Tips for Effective Diabetes Management with Insulin Shots
Managing diabetes with insulin shots requires careful attention to various aspects of treatment. Here are five essential tips to optimize the use of insulin shots and achieve successful blood sugar control:
Tip 1: Adhere to the Prescribed Regimen
Follow the insulin dosage, timing, and injection technique as prescribed by your healthcare provider. Consistency in insulin administration is crucial for maintaining stable blood sugar levels.
Tip 2: Monitor Blood Sugar Regularly
Regular blood sugar monitoring provides valuable insights into the effectiveness of insulin shots. Monitor your blood sugar levels as recommended by your healthcare provider to identify patterns and make necessary adjustments to your insulin regimen.
Tip 3: Manage Carbohydrate Intake
Carbohydrates have a significant impact on blood sugar levels. Learn to estimate carbohydrate content in foods and adjust your insulin dose accordingly. A balanced diet that considers carbohydrate intake can help prevent blood sugar spikes and improve overall glycemic control.
Tip 4: Exercise Regularly
Regular physical activity improves insulin sensitivity, allowing the body to use insulin more effectively. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Tip 5: Pay Attention to Injection Technique
Proper injection technique ensures accurate insulin delivery and minimizes discomfort. Use the correct needle length and injection site, and inject the insulin at a 90-degree angle. Rotate injection sites to prevent lipohypertrophy (fatty lumps).
These tips can empower individuals with diabetes to take an active role in their own health management and optimize the use of insulin shots for effective blood sugar control.
Conclusion: Adhering to these tips can contribute to improved diabetes management outcomes, reducing the risk of complications and enhancing overall well-being.
Conclusion
In conclusion, “shots for diabetes,” or insulin injections, play a vital role in regulating blood sugar levels and preventing complications in individuals with diabetes. Effective diabetes management with insulin shots involves adhering to the prescribed regimen, monitoring blood sugar regularly, managing carbohydrate intake, engaging in regular exercise, and paying attention to proper injection technique.
By following these essential tips, individuals with diabetes can optimize the use of insulin shots, achieve successful blood sugar control, and improve their overall health and well-being. Empowering individuals with the knowledge and skills for effective diabetes management is crucial for reducing the risk of complications and promoting a better quality of life.
Youtube Video: