Diabetes injections are a form of insulin therapy used to manage blood sugar levels in people with diabetes. These injections typically contain fast-acting, short-acting, intermediate-acting, or long-acting insulin, which work to replace or supplement the body’s natural insulin production.
Insulin is a hormone that helps glucose, or sugar, enter cells for energy production. In people with diabetes, the body either does not produce enough insulin or does not use insulin effectively, leading to high blood sugar levels. Diabetes injections provide a controlled dose of insulin to help regulate blood sugar levels, preventing complications such as nerve damage, kidney disease, and heart disease.
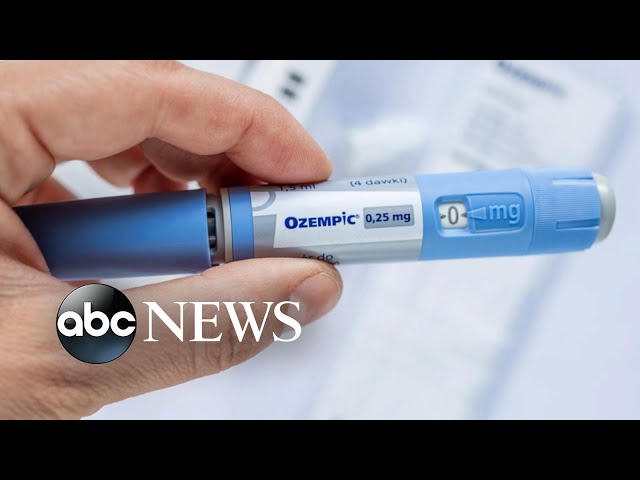
There are various types of diabetes injections available, including pens, syringes, and pumps. The type of injection depends on the individual’s needs and preferences. Regular monitoring of blood sugar levels is crucial to ensure optimal insulin dosage and prevent complications.
Diabetes Injections
Diabetes injections are a crucial aspect of diabetes management. They provide essential insulin to regulate blood sugar levels, preventing complications and improving overall health outcomes.
- Insulin Delivery: Injections deliver insulin directly into the body, mimicking the pancreas’s natural function.
- Blood Sugar Control: Insulin helps glucose enter cells, lowering blood sugar levels and preventing hyperglycemia.
- Complication Prevention: Injections reduce the risk of long-term complications such as nerve damage, kidney disease, and heart disease.
- Convenience and Flexibility: Injections come in various forms (pens, syringes, pumps), allowing for convenient and personalized administration.
- Monitoring and Adjustment: Regular blood sugar monitoring helps adjust insulin dosage, ensuring optimal control.
- Education and Support: Healthcare professionals provide education and support to empower individuals to manage their injections effectively.
In summary, diabetes injections are vital for managing blood sugar levels, preventing complications, and improving the quality of life for people with diabetes. They involve insulin delivery, blood sugar control, complication prevention, convenience, monitoring, and ongoing education. Understanding these key aspects is essential for effective diabetes management and long-term well-being.
Insulin Delivery
Insulin delivery is a crucial component of diabetes injections, as it replaces or supplements the body’s natural insulin production. In healthy individuals, the pancreas releases insulin in response to blood sugar levels, allowing glucose to enter cells for energy production. However, in people with diabetes, the pancreas either does not produce enough insulin or does not use insulin effectively, resulting in high blood sugar levels.
Diabetes injections provide a controlled dose of insulin to mimic the pancreas’s function. By delivering insulin directly into the body, injections help regulate blood sugar levels, preventing hyperglycemia and its associated complications. The various types of diabetes injections (pens, syringes, pumps) allow for personalized insulin delivery, ensuring optimal blood sugar control and reducing the risk of long-term health issues.
Understanding the importance of insulin delivery in diabetes injections empowers individuals to effectively manage their condition. Regular blood sugar monitoring and adherence to prescribed injection schedules are essential for maintaining blood sugar levels within a healthy range. Healthcare professionals play a vital role in educating and supporting individuals, ensuring they have the knowledge and skills to administer injections properly and adjust insulin dosage as needed.
Blood Sugar Control
Blood sugar control is a fundamental aspect of diabetes management, and diabetes injections play a vital role in achieving this control. Insulin, delivered through injections, helps glucose enter cells, effectively lowering blood sugar levels and preventing hyperglycemia, a condition characterized by abnormally high blood sugar.
Elevated blood sugar levels can lead to a cascade of health complications, including nerve damage, kidney disease, and cardiovascular problems. Diabetes injections, by maintaining blood sugar levels within a healthy range, help prevent these complications and promote overall well-being.
Understanding the connection between blood sugar control and diabetes injections is crucial for effective diabetes management. Regular blood sugar monitoring and adherence to prescribed injection regimens are essential for maintaining optimal blood sugar levels.
Healthcare professionals play a vital role in educating individuals with diabetes on the importance of blood sugar control and the proper use of diabetes injections. This education empowers individuals to manage their condition effectively, reducing the risk of complications and improving their quality of life.
Complication Prevention
Diabetes injections play a crucial role in preventing long-term complications associated with diabetes, including nerve damage, kidney disease, and heart disease. These complications can significantly impact individuals’ quality of life and overall health.
Uncontrolled blood sugar levels, a characteristic of diabetes, can damage blood vessels and nerves over time. Nerve damage, or neuropathy, can lead to numbness, pain, and weakness in the hands, feet, and legs. Diabetic kidney disease, or nephropathy, can impair kidney function and potentially lead to kidney failure. High blood sugar levels can also contribute to the development of heart disease, increasing the risk of heart attacks and strokes.
Diabetes injections, by maintaining blood sugar levels within a healthy range, help prevent or delay the onset and progression of these complications. Insulin, delivered through injections, allows glucose to enter cells, reducing blood sugar levels and minimizing the damage caused by hyperglycemia.
Understanding the connection between diabetes injections and complication prevention is essential for effective diabetes management. Adherence to prescribed injection regimens and regular blood sugar monitoring are crucial for maintaining optimal blood sugar control and reducing the risk of long-term complications.
Healthcare professionals play a vital role in educating individuals with diabetes about the importance of complication prevention and the proper use of diabetes injections. This education empowers individuals to manage their condition effectively, improving their overall health outcomes and quality of life.
Convenience and Flexibility
The convenience and flexibility offered by diabetes injections contribute significantly to effective diabetes management. The availability of various injection forms (pens, syringes, and pumps) allows individuals to choose the method that best suits their needs and lifestyle.
- Discretion and Portability: Pens and syringes are compact and discreet, enabling individuals to administer injections privately and conveniently throughout the day.
- Dose Customization: Pens and syringes allow for precise dose adjustments, ensuring that individuals receive the exact amount of insulin they need.
- Technological Advancements: Insulin pumps offer continuous insulin delivery, providing more precise blood sugar control and reducing the need for multiple daily injections.
- Personalized Therapy: The range of injection options empowers individuals to work with their healthcare providers to create a personalized injection plan that fits their specific needs and preferences.
The convenience and flexibility of diabetes injections not only enhance the quality of life for individuals with diabetes but also contribute to better disease management. By enabling discreet, customizable, and personalized insulin delivery, diabetes injections empower individuals to take an active role in their health and achieve optimal blood sugar control.
Monitoring and Adjustment
Monitoring and adjustment are essential aspects of diabetes injections, as they enable individuals to personalize their insulin therapy and achieve optimal blood sugar control. Regular blood sugar monitoring provides valuable feedback on how the body is responding to insulin injections, allowing for timely adjustments to ensure effective management of diabetes.
- Assessing Insulin Effectiveness: Blood sugar monitoring helps assess the effectiveness of insulin injections. By tracking blood sugar levels before and after injections, individuals can determine if the insulin dosage is adequate or needs adjustment.
- Identifying Patterns and Trends: Monitoring blood sugar levels over time helps identify patterns and trends. This information can be used to adjust insulin dosage to match the body’s changing insulin needs, such as during periods of increased activity or illness.
- Preventing Hypoglycemia and Hyperglycemia: Regular blood sugar monitoring helps prevent both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). By detecting blood sugar trends, individuals can adjust insulin dosage to avoid extreme fluctuations and maintain stable blood sugar levels.
- Empowering Self-Management: Monitoring and adjustment empower individuals to take an active role in managing their diabetes. By understanding how their body responds to insulin injections, they can make informed decisions about dosage adjustments, promoting self-reliance and improving overall diabetes management.
The connection between monitoring and adjustment and diabetes injections is crucial for achieving optimal blood sugar control. By regularly monitoring blood sugar levels and making necessary adjustments to insulin dosage, individuals can effectively manage their diabetes, reduce the risk of complications, and improve their quality of life.
Education and Support
Education and support are integral components of effective diabetes management, particularly in the context of diabetes injections. Healthcare professionals play a crucial role in educating individuals about the proper use of diabetes injections, empowering them to take an active and informed role in their self-care.
This education and support encompass various aspects, including:
- Injection Techniques: Healthcare professionals provide comprehensive training on the proper techniques for injecting insulin, ensuring safe and effective administration.
- Blood Glucose Monitoring: Individuals are educated on the importance of regular blood glucose monitoring to assess the effectiveness of insulin injections and adjust dosages as needed.
- Insulin Adjustment: Healthcare professionals guide individuals in understanding how to adjust insulin dosage based on blood glucose levels, activity level, and diet.
- Lifestyle Management: Education includes guidance on healthy eating habits, regular exercise, and stress management to complement diabetes injections and improve overall health.
- Emotional Support: Healthcare professionals provide emotional support and encouragement, recognizing the challenges individuals may face in managing their diabetes.
The practical significance of this education and support is immense. By empowering individuals with the knowledge and skills to manage their diabetes injections effectively, healthcare professionals contribute to:
- Improved Blood Glucose Control: Proper injection techniques and dosage adjustments help individuals maintain optimal blood glucose levels, reducing the risk of complications.
- Reduced Risk of Hypoglycemia and Hyperglycemia: Education on blood glucose monitoring and insulin adjustment empowers individuals to prevent extreme blood glucose fluctuations.
- Enhanced Self-Management: Individuals gain confidence and independence in managing their diabetes, promoting self-reliance and well-being.
- Improved Quality of Life: Effective diabetes management through injections allows individuals to lead active and fulfilling lives, reducing the impact of diabetes on their daily routine.
In conclusion, education and support provided by healthcare professionals are essential for effective diabetes injections. By empowering individuals with the necessary knowledge and skills, healthcare professionals play a vital role in improving blood glucose control, reducing the risk of complications, and enhancing the quality of life for individuals with diabetes.
FAQs on Diabetes Injections
Diabetes injections play a crucial role in managing blood sugar levels for individuals with diabetes. Understanding the purpose, benefits, and administration of diabetes injections is essential for effective diabetes management. This FAQ section addresses common questions and concerns related to diabetes injections, providing concise and informative answers.
Question 1: What is the purpose of diabetes injections?
Answer: Diabetes injections deliver insulin into the body, mimicking the pancreas’s natural function of regulating blood sugar levels. Insulin helps glucose enter cells for energy production, preventing high blood sugar levels and associated complications.
Question 2: Are diabetes injections painful?
Answer: Modern insulin injection devices are designed to minimize discomfort. The needles used are very fine, and injection techniques can be taught to reduce pain. Most individuals experience little to no pain during injections.
Question 3: How often do I need to take diabetes injections?
Answer: The frequency of diabetes injections varies depending on the type of insulin used and individual needs. Some people may require multiple injections per day, while others may need injections only once or twice a day. Healthcare professionals will determine the appropriate injection schedule based on individual circumstances.
Question 4: Can I travel with diabetes injections?
Answer: Yes, traveling with diabetes injections is possible. It is important to store insulin properly during travel, keep it cool and protected from extreme temperatures. Individuals should also carry a doctor’s note explaining the need for injections and any additional supplies, such as syringes or insulin pumps.
Question 5: What are the potential side effects of diabetes injections?
Answer: Diabetes injections are generally safe, but some potential side effects include skin reactions at the injection site, low blood sugar (hypoglycemia), and weight gain. Proper injection techniques and regular monitoring of blood sugar levels can help minimize these side effects.
Question 6: How can I learn to administer diabetes injections?
Answer: Healthcare professionals, such as doctors or nurses, provide comprehensive training on how to administer diabetes injections safely and effectively. They will demonstrate the proper injection technique, discuss storage and handling of insulin, and answer any questions.
Summary of key takeaways or final thought:
Diabetes injections are an essential part of diabetes management, helping individuals regulate blood sugar levels and prevent complications. Understanding the purpose, benefits, and administration of diabetes injections is crucial for effective self-care. By working closely with healthcare professionals, individuals can learn the necessary skills and knowledge to manage their diabetes injections confidently and effectively.
Transition to the next article section:
In the next section, we will discuss the benefits of diabetes injections and how they contribute to overall diabetes management.
Diabetes Injections
Diabetes injections play a vital role in regulating blood sugar levels and preventing complications for individuals with diabetes. Here are some essential tips to optimize the use of diabetes injections:
Tip 1: Proper Injection Technique
Follow the instructions provided by your healthcare professional for the correct injection technique. Ensure you inject at the right angle, rotate injection sites, and store insulin appropriately to maintain its effectiveness.
Tip 2: Regular Blood Sugar Monitoring
Monitor your blood sugar levels regularly as directed by your healthcare team. This will help you understand how your body responds to insulin and make necessary dosage adjustments.
Tip 3: Meal Planning and Insulin Timing
Plan your meals and snacks around your insulin injections to ensure optimal blood sugar control. Consider the carbohydrate content of your food and adjust your insulin dosage accordingly.
Tip 4: Exercise Management
Regular exercise can affect blood sugar levels. Inform your healthcare team about your exercise routine and adjust your insulin dosage or meal plan as needed to prevent hypoglycemia.
Tip 5: Travel Considerations
When traveling, store your insulin properly and carry a doctor’s note explaining your need for injections. Consider time zone changes and pack extra supplies to avoid disruptions in your injection schedule.
Tip 6: Emotional and Social Support
Managing diabetes can be challenging. Seek support from family, friends, or support groups to cope with the emotional aspects of living with diabetes and stay motivated.
Tip 7: Technology and Innovation
Take advantage of advancements in diabetes management technology, such as continuous glucose monitors and insulin pumps. These devices can provide real-time data and automate insulin delivery, improving blood sugar control.
Tip 8: Regular Follow-Up Appointments
Attend regular follow-up appointments with your healthcare team to review your diabetes management plan, adjust medications, and monitor your overall health.
Summary:
By following these tips, individuals using diabetes injections can effectively manage their blood sugar levels, reduce the risk of complications, and improve their overall well-being. Remember, diabetes management is an ongoing journey, and working closely with your healthcare team is essential for achieving optimal outcomes.
Transition to the article’s conclusion:
In conclusion, diabetes injections are a crucial aspect of diabetes management, and using them effectively requires proper technique, regular monitoring, careful planning, and ongoing support. By adhering to these tips and working with your healthcare team, you can optimize your diabetes management and live a full and healthy life.
Conclusion
Diabetes injections have revolutionized diabetes management, providing individuals with a means to regulate blood sugar levels and prevent complications. Through the exploration of their purpose, benefits, administration, and essential tips for effective use, this article has highlighted the significance of diabetes injections in empowering individuals to take control of their diabetes.
Diabetes injections are not merely a treatment but a tool for individuals to live full and healthy lives. By understanding the principles of diabetes injections and working closely with healthcare teams, individuals can optimize their diabetes management, reduce the risk of complications, and achieve improved overall well-being. The future of diabetes injections holds promise, with ongoing research and technological advancements aiming to further enhance their effectiveness and convenience.
Youtube Video: